Physical Therapy For Knee Pain Glendale AZ
Knee Pain?
Osteoarthritis
Anatomy
Arthritis is most easily defined as normal “wear and tear” on the joint over the years. As we age, the health of the cartilage and the capsule that surrounds our knee joint degrades. There is reduced fluid to lubricate the joint, muscle weakness reduces optimal alignment of the joint and cartilage wears down or thins causing the underlying bone to take more stress. Most often, the medial compartment of the knee is affected compared to the outside portion of the joint do to its anatomical structure and the shape of our leg, the cartilage is like the tread on a tire, the inside portion of the tread typically wears quicker unless the alignment is in a unique position.
Who is at risk
Knee arthritis is more common in women verses men, increasing frequency with age. Risk factors vary from genetic predisposition and bone health to high impact athletes or joint trauma. Obesity also increases the risk of knee arthritis due to the constant excess loading on the joint with daily activities. Sedentary lifestyle does not help the cartilage either, infact, once your cartilage begins to degrade, you want to continue moving the joint through full range of motion and provide it with compressive stresses to help keep the cartilage healthy.
How Pt can help
Physical therapy will address knee arthritis with both manual and exercise driven interventions. Stretching of the tissues surrounding the knee typically reduces pain and overall inflammation, which allows better participation and tolerance to strengthening exercises targeting joint alignment and stability. Our goal is to reduce your overall pain and improve your function, helping to avoid a large orthopedic surgery if possible. We can also assist in guiding you through the progressive treatments of knee arthritis in regards to PT, corticosteroid injections, hyaluronic acid injections (gel), meniscus surgeries, partial joint replacements and full joint replacement.
Total Knee Arthroplasty
Anatomy
A total joint replacement occurs when the cartilage that protects the bony surfaces within a joint thins (arthritis), resulting in irritation and inflammation within the joint capsule. Convservative treatment can delay the thinning of the cartilage and give you improved quality of life, if conservative treatment is no longer helping, a surgeon will choose the next treatment progression, the end result of end stage arthritis is a joint replacement. Replacing the components of the joint eliminates the osteoarthritis which is what causes the thinning of the cartilage.
Who is at risk
Arthritis progresses as we age, risk factors are obesity, smoking, cutting type sports when we are young, trauma, meniscus tears, poor strength and range of motion about the knee and changes in gait pattern.
How Pt can help
Physical therapy is imperative following a joint replacement as it is of the utmost importance to reduce inflammation, guide incisional healing, restore range of motion and begin strengthening the musculature surrounding the new joint. Typically, expect to complete at least 8-12 weeks of physical therapy following your surgery to maximize the benefit from your new joint. It takes a full 12 months to recover fully.
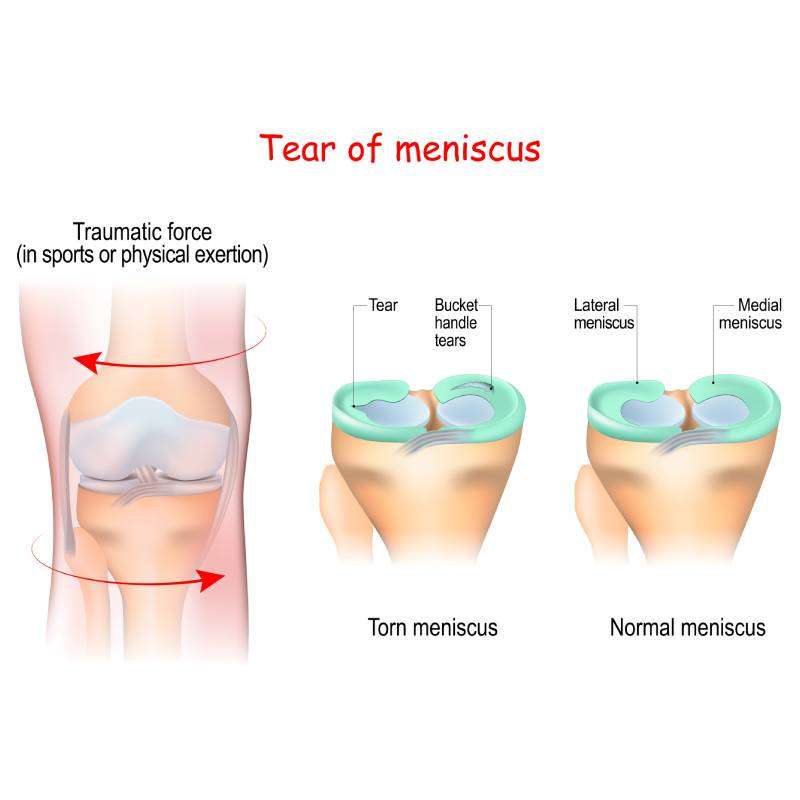
Meniscus Tear/Repair
Anatomy
The menisci are two cartilaginous structures in each knee, they sit at the top of your shin bone and they help to deepen the socket that your femur sits in, this gives slight stability to your knee. This cartilage is very good at accepting compression forces when we run, however, it struggles to accept sheer forces across its surface. We see an increased incidence of meniscus tears in the second and third decade as a result of reduced blood supply causing cartilage to become more brittle and therefore more susceptible to tears at this age. There are two main categories of tears, acute and degenerative. Within those two types of tears there are 10-20 different forms of tears and these variables affect the management of the injury. We see a higher prevalence of acute tears in athletes in their 20’s and 30’s. We see a larger number of degenerative tears in middle to late years, once the meniscus has begun to degrade it is imperative to see a Physical Therapist to work on maintaining your joint stability, surrounding strength and knee range of motion to prevent further stress to the underlying articular cartilage.
Who is at risk
We are at risk for acute tears in our 20’s and 30’s and degenerative tearing in our middle decades of life. We see a prevalence of 12-14% and slightly higher frequency in women versus men. Active individuals who participate in twisting and cutting type sports are at highest risk of damaging the meniscus.
How PT can help
We perform a thorough evaluation to determine if your meniscus is torn or if there is other underlying damage causing your pain. If the meniscus is torn PT is the standard of care in today’s medical options. We are able to provide knee stability, reduction of pain and avoid surgery in approx 70% of patients.
ACL Tear
Anatomy
The anterior cruciate ligament is a primary stabilizer of your knee, it runs from the femur to the tibia in a diagonal posterior lateral to anterior medial direction. The biomechanical function is multifactorial and complex. It helps to resist your lower leg (tibia) from shifting anterior and rotating too far in multiple directions as we run, cut, jump. ACL injuries depend on several factors:
• The patient’s gender (females vs. males)
• The demands of the patient’s profession
• The presence of previous ligament damage.
• Congenital Ligament Laxity
An injury to the ACL can lead to instability of the knee and may increase the rate of articular cartilage breakdown.
Who is at risk
Approximately 100,000 individuals injure their anterior cruciate ligament (ACL) each year in the United States. The costs, including surgical intervention and rehabilitation, can approach $20,000. However, these figures do not include potential long-term consequences of articular cartilage changes. The rates of injury differ between males and females, with the females injuring their ACLs anywhere from 2 to 9 times more often than their male counterparts. Sports such as soccer, basketball, volleyball, and gymnastics all demonstrate higher rates of ACL injuries in females than males. Gender differences in ACL injuries are multifactorial and may result from a combination of neuromuscular, biomechanical, and structural/hormonal factors. An ACL injury usually occurs as a result of an acute trauma involving a valgus and external rotation force applied to the knee while the foot is planted (sometimes a direct force, but not usually). Damage may also result from excessive internal rotation with hyperextension of the knee. Injuries are frequently non-contact and occur during the deceleration phase of absorption accompanied by contraction of the quadriceps muscle. In certain situations, an initial injury can partially tear the ACL and a subsequent injury can “finish off” the remaining intact ligamentous fibers.
The extent of swelling may vary depending on the patient and what part of the ligament was torn (some areas are more highly vascularized than others).
How PT can help
The majority of ACL tears will be treated with surgical intervention, most commonly a reconstruction with either the patients tissue (autograft), or cadaver tissue (allograft), this tissue comes from one of the hamstring, patellar tendon, or quad tendons. The ACL is reconstructed with tunnels that are drilled in the femur and tibia and placing the new tissue in the knee to provide stability. The rehabilitation after an ACL reconstruction is extensive.
◦ At Wall 2 Wall Sports & Rehab we have world class education and experience treating ACL reconstructions on all athlete levels and all types of reconstructions.
◦ The current literature supports a minimum rehabilitation course of 9 months, as long as the individual meets all objective criteria based goals through the rehab process. Our rehab program follows a 4 stage evidence based system that is time and criterion based to allow our athletes to return to sport safely.
◦ We currently use the Vail Sport Cord Test as well as a cluster of other testing to return our athletes back to sport like activities. We work closely with coaches and athletic trainers in this process.
What are the signs and symptoms of an acute ACL injury?
Pain
Pain may be present with weight-bearing or end-ranges of motion secondary to swelling which distends the joint capsule.
Giving Way

Noise
a “snap” or Pop” at the time of injury is usually reported.
Limited Range of Motion
Swelling
Patellofemoral Pain
Anatomy
Patellofemoral pain syndrome (PFPS) is pain reported in the front part of the knee, usually under or around the knee cap. This is typically caused by an imbalance of the quadriceps pull on the knee cap, causing abnormal pressure or joint tracking. This can be caused by a muscle imbalance, anatomical knee joint position or weak hips resulting in a knee collapse. Unfortunately, untreated PFPS can lead to patellofemoral arthritis later in life. The pain generated by this pathology can be debilitating.
Who is at risk
This injury is one of the more commonly reported conditions in active individuals, more often in women compared to men. Common risk factors include reduced knee flexion during jumping activities, asymmetrical hip weakness, and impaired muscular endurance as fatigue leads to poor joint alignment. This pathology is very common in runners and other endurance type athletes.
How PT can help
During the evaluation, we use special testing to help clinically diagnose PFPS versus an array of other knee pathologies, including joint measurements and muscle strength testing, manual manipulation of the knee cap and neuromuscular training. Depending on the cause of the pain, we target exercises to strength and better maintain knee position with all activities, including jumping and running